The integration of artificial intelligence (AI) into primary care is no longer a futuristic concept—it’s here. With the recent NICE early value assessment (HTE24) guidance focusing on AI for assessing and triaging suspicious skin lesions, GPs are now at the forefront of a major shift in dermatology care.
But what does this mean for your day-to-day practice? Could AI tools help cut NHS waiting times? And what do GPs need to make this work in real life?
Let’s break it down.
What Is NICE HTE24 All About?
The HTE24 guidance from NICE evaluates emerging AI-based technologies that analyse images of skin lesions and help determine their risk of malignancy. These systems are not designed to replace clinical judgment but to support it, especially in the urgent suspected skin cancer (2-week wait) pathway [1].
Key takeaway: AI tools could offer earlier identification and better prioritisation of potential cancers—before the patient even reaches a specialist.

Why This Matters Now: The NHS Waiting List Crisis
NHS dermatology is under pressure, and GPs are often stuck in the middle. As of early 2025, median NHS treatment waiting times stood at 14.2 weeks, nearly double the 7.5-week median in early 2020 [2]. Skin cancer referrals have increased by 22% since 2019 [3], overwhelming specialist services and leading to delays in diagnosis and treatment.
AI triage tools can help reduce inappropriate referrals, flag high-risk patients faster, and ease the burden on dermatologists—potentially cutting time-to-diagnosis and improving outcomes.
How the DERM AI Tool Works in Practice
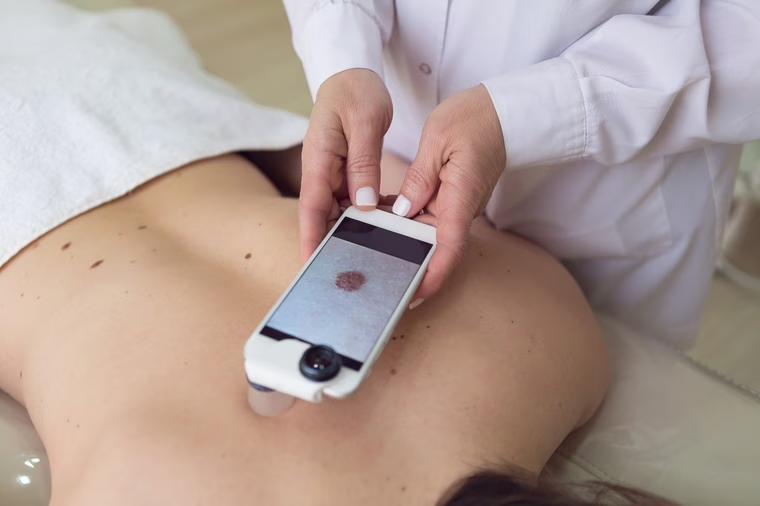
DERM is an AI-powered skin lesion assessment tool evaluated under NICE HTE24. It is designed to support the urgent skin cancer referral pathway by helping healthcare professionals determine whether a lesion is cancerous, pre-cancerous, or benign.
Here’s how it works step-by-step:
-
1. AI Assessment
The DERM system analyses skin lesion images and classifies them based on cancer risk. It’s used for adults aged 18 or over. -
2. Virtual Dermatologist Review
If the lesion is flagged as potentially cancerous or pre-cancerous, an NHS dermatologist reviews the case remotely and recommends the next steps in care. -
3. Extra Safeguards for Skin of Colour
For patients with black or brown skin, an additional review by another healthcare professional is carried out during the current evidence generation period. This extra step is due to the lower incidence of skin cancer in these groups and the need for stronger evidence of accuracy. -
4. Benign Lesions Discharged
If DERM identifies the lesion as benign, the patient is discharged from the urgent pathway. They receive written advice and reassurance from a healthcare professional, helping to reduce unnecessary stress and appointments. -
5. Flexibility in Use
DERM can be used with or without further review for lesions identified as non-cancer, offering flexibility based on local clinical pathways and clinician confidence.

What Are the Benefits for GPs?
- Better Decision-Making Support
Think of AI as a clinical assistant: it doesn’t replace you but gives a “second opinion” that can boost confidence in uncertain cases, especially in under-resourced areas with limited dermatology access.
- Prioritised Referrals
By accurately identifying high-risk lesions, these systems help GPs make more focused referrals, increasing the chance that urgent cases are seen within target timelines.
- Reduced Admin Burden
Unnecessary 2WW referrals create admin work and stress for GPs. Smarter triage could save time and free you up for more value-added consultations.
What GPs Need to Make This Work
Training and Upskilling
AI tools must be embedded into clinical workflows, not bolted on. GPs will need training in dermatology triage, digital imaging, and understanding AI limitations.
Infrastructure and Interoperability
To benefit from AI, practices will need secure, NHS-compliant image capture systems, compatible with EMIS or SystmOne. Integration with referral systems is also key.
Governance and Clarity
There must be clear governance around how AI is used, who is accountable, and how performance is monitored. Practices need reassurance that using these tools is safe, ethical, and clinically justified.
Potential Challenges to Address
While the guidance is promising, NICE recognises that more evidence is needed to confirm long-term clinical impact and cost-effectiveness [1]. Currently, some tools are being piloted but not yet recommended for widespread rollout. So, GPs should stay informed and be ready to adopt as more robust data emerges.
What’s Next? Preparing for AI-Supported Dermatology
This isn’t just about technology—it’s about rethinking dermatology pathways to create faster, smarter, and more patient-centred care. If implemented correctly, AI could help us:
- Reduce waiting lists
- Improve early detection of skin cancer
- Empower GPs with better diagnostic tools
- Free up secondary care capacity for complex cases
GPs play a pivotal role. Engaging with these tools early could help shape how they’re used in primary care.
Final Thoughts
AI in dermatology is one of the most exciting changes in primary care—and HTE24 puts us on the path to adopting it safely and sensibly. As the evidence base grows, GPs will be key to evaluating how AI can improve access, accuracy, and efficiency in skin cancer care.
References
- National Institute for Health and Care Excellence. (2024). HTE24: AI technologies for assessing skin lesions. NICE Early Value Assessment Guidance. Retrieved from: https://www.nice.org.uk/guidance/hte24
- British Medical Association. (2025). NHS backlog data analysis: waiting times overview. Retrieved from: https://www.bma.org.uk/advice-and-support/nhs-delivery-and-workforce/pressures/nhs-backlog-data-analysis
- NHS Digital. (2024). Monthly Cancer Waiting Times Statistics. Retrieved from: https://digital.nhs.uk/data-and-information/publications/statistical/cancer-waiting-times
